Vermox Versus Albendazole: Which Anthelmintic Wins?
Mechanisms of Action: How They Kill Worms
In the gut, two stalwart anthelmintics attack parasites by crippling their internal scaffolding. Albendazole and mebendazole bind parasite β‑tubulin, destabilizing microtubules and blocking glucose uptake, wich starves worms and halts egg production.
Albendazole is converted to an active sulfoxide that reaches tissue parasites, giving systemic reach against larval stages; mebendazole largely stays luminal, exerting powerful local effects but limited systemic activity. Teh result is different clinical uses.
Both drugs immobilize and kill worms by energy depletion and mitotic arrest; variable species susceptibility and parasite location guide the clinically optimal choice.
Spectrum of Activity: Which Parasites They Target

Clinically, vermox often treats intestinal worms while albendazole reaches tissue-dwelling parasites because of better systemic absorption. Teh difference shapes which infections respond best to each drug.
Vermox excels against Enterobius (pinworm), Ascaris, Trichuris and various hookworms in gut-limited infections. Albendazole covers those too but adds activity against neurocysticercosis and echinococcosis when given appropriately.
Efficacy varies: single-dose mebendazole may clear pinworms, but Trichuris infections are tougher; albendazole's systemic reach makes it preferable for larval stages or tissue cysts, especially under specialist guidance.
Public health programs use both: vermox for school-based mass deworming, albendazole for campaigns targeting multiple parasitic diseases. Occassionally, combination strategies are used to broaden control. Decisions also reflect resistance patterns, availability and patient comorbidities.
Efficacy and Clinical Evidence Compared Side by Side
Clinical trials and real-world studies paint a nuanced picture: vermox and albendazole both clear common intestinal worms, but head-to-head outcomes vary by species and regimen, leaving clinicians to balance evidence and practical factors, judgment too.
Meta-analyses show albendazole often outperforms in treating hookworm and giardia, while vermox (mebendazole) shines against pinworms and certain soil-transmitted helminths; direct comparisons are sometimes limited by study heterogeneity. Reported cure rates frequently vary by dosing.
Programmatic use shows single-dose albendazole works well for mass deworming, whereas vermox multi-day courses can increase cure for some infections. Reinfection remains common, and Occassionally repeated treatments are necessary to maintain control in endemic areas.
Resistance remains uncommon but monitored, so safety and tolerability guide choice: albendazole can be teratogenic in animal studies, vermox profiles are generally mild. Clinicians also weigh availability, cost, and patient ability to aquire medication convenience.
Safety Profiles: Side Effects, Pregnancy, and Contraindications

In clinical practice the safety trade offs often frame the choice. Common adverse effects are usually mild, such as nausea, abdominal pain, headaches or dizziness, but rare serious events can change management. vermox tends to cause transient GI complaints and occasional alopecia, while albendazole is linked more often with elevated liver enzymes and, rarely, bone marrow suppression. Teh patient’s baseline labs and medication list set the stage.
Pregnancy is a pivotal consideration. Both drugs are typically avoided in early gestation because teratogenicity has been shown in animal studies and human data are limited. Contraception and counselling before treatment are advised, and if therapy is unavoidable specialist input and risk benefit documentation are neccessary.
Monitor routinely.
Dosing, Administration, and Cost Considerations Worldwide
Clinicians balance simplicity and precision when prescribing anthelmintics; single-dose regimens improve adherence, while multi-day courses target tissue-invasive infections. Teh choice often depends on parasite lifecycle, patient age, pregnancy status and drug availability, so pragmatic stewardship matters in low-resource settings.
Oral mebendazole (vermox) is typically 100 mg twice daily for three days or a 500 mg single dose depending on indication; albendazole schedules vary. Administration with fatty meals increases albendazole absorption, altering efficacy. Stockouts, generic pricing and national formularies shape what patients actually recieve.
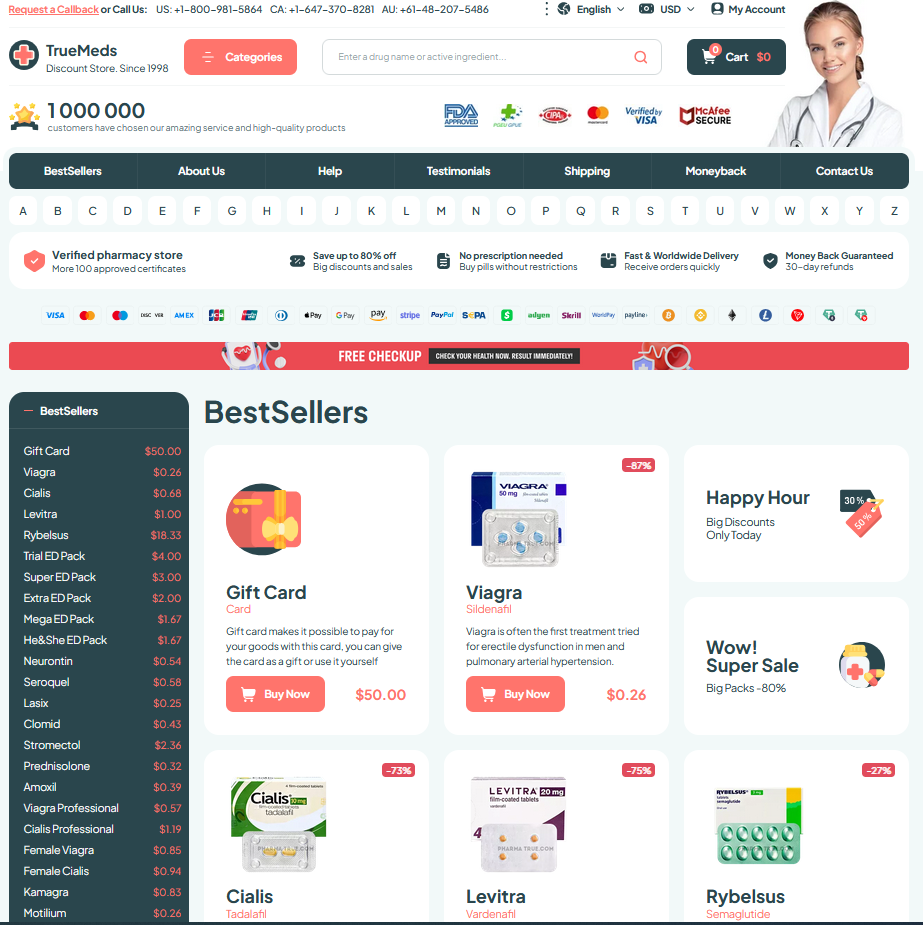
Cost varies: mass-treatment programs often procure mebendazole or albendazole cheaply, whereas retail prices reflect brand, packaging and distribution. Example price snapshot follows:
| Region | Typical price | Notes |
|---|---|---|
| Low-income | $0.10 | Public programs often free |
| Middle-income | $0.5-2 | Retail margins vary |
| High-income | $5-10 | Brand premiums apply |
Choosing Wisely: Patient Factors Guiding Drug Selection
Start with the parasite: mebendazole favors intestinal nematodes like pinworms and whipworms, while albendazole covers a broader range including tissue parasites; epidemiology and local resistance shape the choice plus context.
Patient factors matter: age, pregnancy status, hepatic disease and drug interactions often tip preference. For example, pregnant women in first trimester may avoid albendazole, and children require weight-based dosing Wich
Finally, access, cost and dosing convenience influence choice: single-dose mebendazole improves adherence in low-resource settings, while albendazole might suit systemic infections; shared decision-making ensures best individual care and follow-up plans. Vermox (mebendazole) label - DailyMed Mebendazole - NCBI Bookshelf